Prostate cancer cellular immunotherapy
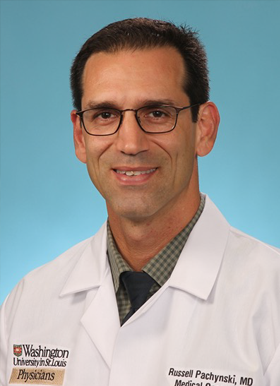
Russell Pachynski, MD, Associate Professor of Medicine, Division of Oncology, Director of Genitourinary (GU) Oncology Research, Washington University School of Medicine in St. Louis, published a paper in Cancer Immunology Research (“High dimensional analyses reveal activation of lymphocyte subsets and reversal of immunoresistance by cytokine-enhanced cellular vaccine therapy in prostate cancer”) examining the only FDA-approved prostate cancer cellular immunotherapy. (Immunotherapy involves stimulating the immune system to fight cancer.)
Cellular Immunotherapy
One promising form of immunotherapy, termed “cellular immunotherapy”, utilizes the patient’s own immune cells and has been used to treat several different cancer types. Cellular immunotherapy has been FDA-approved for prostate cancer since 2010. More recently there have been several other approvals for leukemia, lymphoma, and multiple myeloma. These newer versions incorporate a “chimeric antigen receptor” that targets the tumor cells, and are thus called CAR-T cells. Here, the patient’s T-cells (a type of immune cell) are taken out, modified, activates, and returned to the patient.
Our cellular therapy in prostate cancer utilizes a similar, but less advanced approach as it was developed close to 20 year ago and FDA approved in 2010. What happens with this therapy, which is called Sipuleucel-T (the brand name is Provenge), is that a fraction of the immune cells are removed from the patient (in a process call leukapheresis) similar to the CAR-T approach. However, after removal from the patient the immune cells are not genetically modified with a “CAR” but are stimulated and activated using a modified prostate cancer protein. These activated, “educated” immune cells are then infused back into the patient.
This process is done three times in total, usually about two weeks apart and overall is fairly well tolerated with just minimal flu-like symptoms. Sipuleucel-T (Sip-T) improves survival of these metastatic prostate cancer patients by over four months, with is comparable with all the other approved products and drugs we have for these patients.
“Sip-T, even though it improves the survival of patients, does not do a great job of shrinking the cancer or reducing the PSA, which we use to figure out whether a drug is working. If the tumor shrinks on a CT scan or the PSA levels in the blood down down, we know it’s working. Our work showed that by adding another immunotherapy to Sip-T we can shrink these tumors in mice, and so we are working on turning this into a clinical trial for prostate cancer patients – hopefully we can do the same.”
Pachynski
Unfortunately, the uptate and use of Sip-T has been limited, in part due to the fact that while it does slow down the disease and improve survival – it does not shrink the patient’s tumors on scans or reduce the PSA. We wanted to understand how we could improve this, so we began to study Sip-T in the lab.

The first thing we did was collect, through an IRB-approved protocol, the Sip-T that was leftover from patients after they completed their infusions. After obtaining the patient’s consent, we took the leftover Sip-T and looked at it using an approach called CyTOF (mass cytometry) This is basically a fancy way of looking at all of the different immune cells and being able to not only say which cells are present, but characterize them and see if they are activated or suppressed.
We did this with several patients’ Sip-T products, which had never been done before. Prior to its approval in 2010, when the company was developing it, they had only performed somewhat rudimentary analyses of Sip-T. This surprised us how properly characterized the product itself was, so we decided to do a detailed analysis, which was a big part of the research paper.
Pachynski shares, “These analyses gives us clues as to how we can improve Sip-T. We can randomly throw stuff against the wall and say, combining this or doing that might work, but using the results from the analyses will help us take a more educated approach to making it work better.”
Cytokine Therapy
Another type of immunotherapy is cytokine therapy. Cytokines are small proteins our immunes system uses to communicate and activate immune cells, Based on the potential for cytokines to enhance cellular immunotherapy, we did a clinical trial with Sip-T and the cytokine IL-7.
Results from that multi-center clinical trial (Pachynski et al Journal of ImmunoTherapy for Cancer 2021) showed that combining it with cytokine IL-7 worked better than just the Sip-T alone. In that trial, we saw the PSA come down. We were starting to get a better signal. Based on that trial, we started to see some improvement with IL-7, but then asked the question, okay well there are other cytokines out there in the clinic – could they perform better than IL-7 in combination with Sip-T?
In this paper, we tested several different cytokines and found that the cytokine IL-15 is significantly better then IL-7 in a number of aspects combining it with Sip-T. We then characterized what happens when we added IL-15 to the Sip-T, looking at both how the IL-15 changed the Sip-T, but also how much better it made it kill tumor cells. We then developed a preclinical mouse model of prostate cancer and used these different combinations in the mouse model of prostate cancer.
Pachnyski Lab researchers cut out the tumors and saw more anti-cancer Sip-T cells in the tumors with IL-15 treatment. Additionally by adding IL-15, they reduced some of the immune suppressive effects in the tumor, and shrank the tumors more more effectively.
Sip-T and Clinical Trials
Pachynski has worked with Dendreon, the company that makes Sip-T, and Immunity-Bio which makes an IL-15 drug called N803 which was recently FDA-approved for bladder cancer. Pachynski and one of the first year Oncology fellows, Aashray Singareddy, MD, are currently designing a clinical trial and working on the protocol that will test the combination of Sip-T with N0803 in prostate cancer patients for the first time.
Prostate cancer, in total affects approximately 299,000 men annually. However, the vast majority of that is localized disease, where it has not spread out of the prostate and become metastatic or stage 4, which is about 20 percent of time. There are approximately 35,000 prostate cancer deaths per year from metastatic disease.
We know that even though prostate cancer is, in the localized setting, pretty curable and pretty treatable, once it is metastatic, unfortunately those patients will most likely die from their disease at some point. However, we have good treatment options, but we do not have great immunotherapy options for prostate cancer right now – we’re working to improve this.
Pachynski
Compared to testing a completely new immunotherapy, combining two FDA-approved immunotherapies (Sip-T and N-803) to try and increase efficacy in these patients may be a faster way to improve immunotherapy outcomes in prostate cancer patients.