As a hospitalist, Mark Williams, MD, has spent quite some time considering how we can improve the patient experience, during hospitalization and in the follow-up care once released.
He recently wrote an editorial to an article about the experience of family caregivers in an American hospital as their loved one went through the transition of the ICU to the floor or from the floor back to the ICU.
What it really has to do with is communication with their families/caregivers while in the hospital.

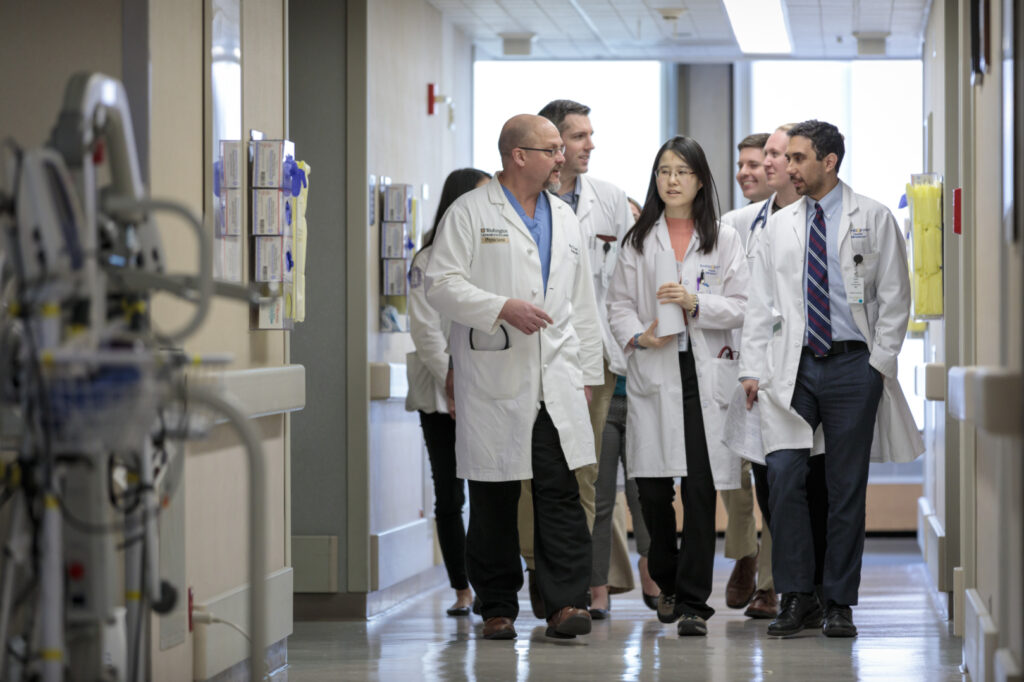
Attempting to understand and enhance communication with hospitalized patients at an academic hospital like Barnes-Jewish Hospital, Dr. Williams collaborated on research on teamwork to improve rounds in the hospital—the century old customary practice of “rounds” in the hospital. By shifting from only the team of physicians (typically a faculty physician, resident, couple of interns and students) to inter-disciplinary rounds the researchers aimed to engage more disciplines involved in a hospitalize patient’s care including: nurses, case managers, social workers, and pharmacists with physicians to meet every morning and talk with one another about the patient’s care and how to move them forward toward hospital discharge.
He wondered how they could do this better and had a unique opportunity while at the University of Kentucky to implement and evaluate an enhanced approach to conducting rounds at the patient’s beside. This eventually evolved into the Interprofessional Team Innovation Model (ITIM). The model was effectively implemented after nine months of piloting and getting everyone onboard. On one thirty-bed unit, two teams (each composed of a hospitalist, nurse case manager and a pharmacist) rounded together daily at the bedside with patients, and their family caregivers if available. Patients and their family caregivers praised the new approach and cost-savings achieved through better patient care financed the extra people. Hospitalists who initially were reluctant, or even opposed, to trying this new approach soon requested to work on these floors. They recognized that teamwork was an “ITIM” of necessity for high quality patient care.
There was a wonderful productivity around having a hospitalist team seeing 15 patients in a day in an academic setting.
Mark Williams, MD, FACP, MHM
Hospital Medicine Division Chief, Professor of Medicine
The success allowed for reduced readmission rates and was propagated across the rest of the hospital and soon won the patient experience award on two different units. Williams shares that this idea stems from visits to Cincinnati Children’s Hospital Medical Center (CCHMC) and learning from Uma Kotagal, MBBS, MSc. She is internationally known for spearheading transformation of Cincinnati Children’s Hospital into a leader in quality improvement for healthcare delivery. Seeing the actions in place got Williams questioning why isn’t this type of rounding everywhere as family-centered rounds are the standard care at children’s hospitals. Learning that St. Louis Children’s Hospital also conducts family-centered rounds sparked the editorial on why this is what needs to be done for not just children but adults. Williams firmly believes there is a responsibility to ensure that patients and their family caregivers are well-informed about the necessary care for the patient once they head home. Involving and including everyone in rounds as well as family member’s means they are on the same page with the same knowledge for care.

Mark Williams has been researching utilization of teamwork in health care for over 15 years and sees the need for care to continue to evolve. Patients evaluated in a subsequent qualitative study emphasized that the most important thing to them is to feel cared for and cared about. Trust is essential in the relationship between the doctor and patient. At Northwestern he worked on setting up a system that when a patient was in the hospital their primary care doctor was always alerted and asked to call the patient to ensure them that they were in good hands with the hospitalist who was caring for them.
Dr. Williams shares, “it was immediately noticeable once that call had been made how it helped bridge the trust between patient and myself. You could see they were now happy I was taking care of them and it was a completely different relationship. We as healthcare professionals have to figure this out so that patients trust us.“
Mark V. Williams, MD, FACP, MHM, is Professor and Chief of the Division of Hospital Medicine and began his collaboration with the Division’s experienced leadership team in October 2021 to build one of the premier academic divisions in the nation. With > 120 physicians and advanced practice clinicians (nurse practitioners and physician assistants), the Division provides care for > 120,000 hospital visits per year. A Past-President of the Society of Hospital Medicine, Founding Editor of the Journal of Hospital Medicine and one of the first 10 Masters in Hospital Medicine, Mark brings his expertise in quality improvement, teamwork, and care transitions to this prestigious institution and talented group.